
Mild Obstructive Sleep Apnea
Sleep is the foundation of our health and well-being, yet for millions […]

What is Overlap Syndrome?
Overlap Syndrome occurs when a person suffers from both Chronic Obstructive Pulmonary […]

Narcolepsy vs. Sleep Apnea
If you find yourself falling asleep during the day, even if you […]
Long-Term Health Issues from Untreated Sleep Apnea
Sleep apnea is a disorder that causes a patient to stop breathing […]

What You Need to Know About CPAP Intolerance
Treating obstructive sleep apnea with continuous positive airway pressure (CPAP) can be […]

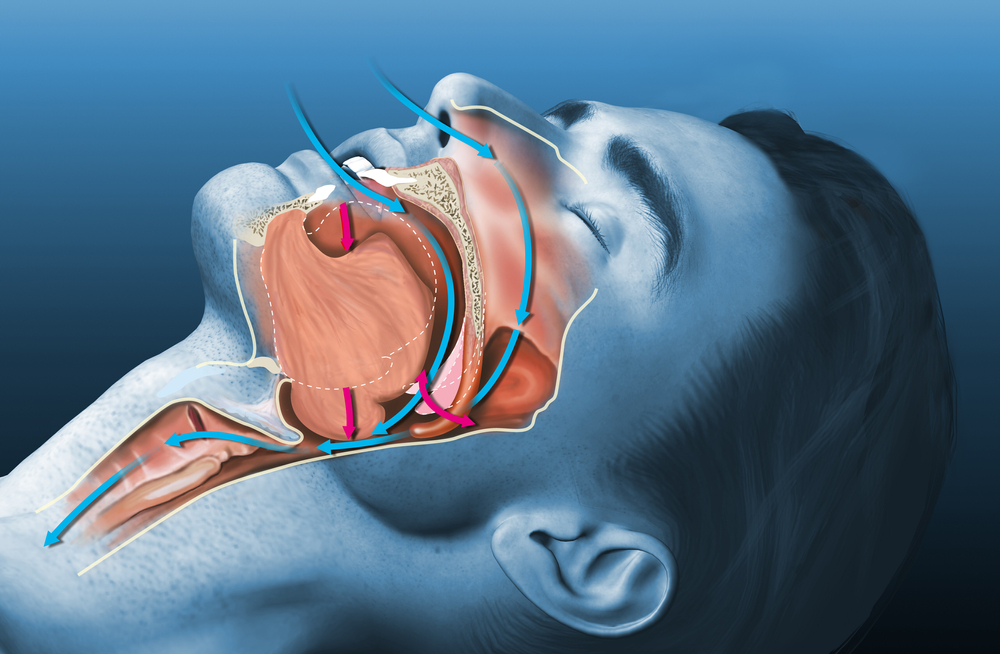
Common Warning Signs of Sleep Apnea
Sleep apnea is a disorder that causes a person to stop and […]

How to Deal with a Snoring Partner
Sleeping is the body’s way of relaxing and recharging for the next […]

Five Reasons Why CPAP Users Should Try Oral Appliances
If you have obstructive sleep apnea, the best treatment for the condition […]

What Is the Best Sleeping Position?
Choosing the best sleeping position is about more than just comfort. If […]

Nocturnal Teeth Grinding Linked to Sleep Apnea
What is Sleep Apnea? Sleep apnea is a sleep disorder that is characterized […]